Congenital heart disease: causes, diagnosis, and treatment

Reviewed by Mike Bohl, MD, MPH, ALM,
Written by Chimene Richa, MD
last updated: Feb 09, 2020
4 min read
Here's what we'll cover
Congenital heart disease (CHD), also called congenital heart defects, is a condition in which a child is born with a structural problem in his or her heart. According to the Centers for Disease Control and Prevention (CDC), almost 1% of all births in the US have congenital heart disease—that’s nearly 40,000 babies per year (CDC, 2019). Heart abnormalities are the most common type of congenital malformation. Furthermore, one in four babies with CHD will have a heart problem that is considered critical CHD. This means that they will likely need a heart procedure sometime during their first year of life (CDC, 2019).
A normal heart has four chambers: two atria (upper chambers) and two ventricles (lower chambers). The wall between the chambers is called the septum, and there are four one-way valves (aortic, pulmonic, mitral, and tricuspid valves) that keep blood flow in the heart from going the wrong way. Lastly, two major arteries come off of the heart. The aorta takes oxygen-rich blood from the left ventricle to the rest of the body. The pulmonary artery carries oxygen-poor blood from the right ventricle to the lungs, where it gets more oxygen.
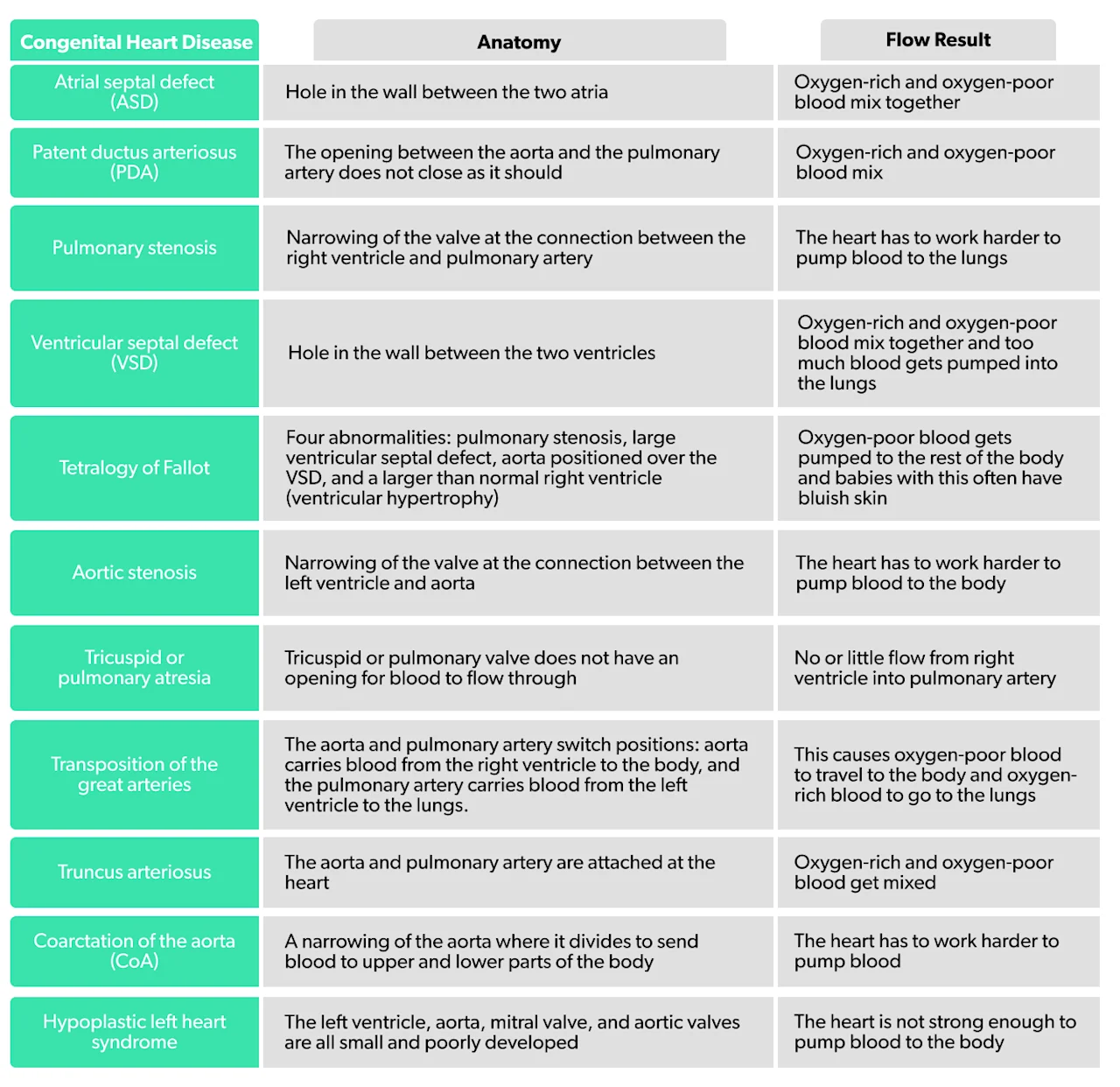
Children can be born with a problem in the walls of the heart, heart valves, or blood vessels, bringing blood to or carrying blood from the heart. The seriousness of the congenital heart disease depends on the structures involved and the child’s symptoms. Some abnormalities do not cause a problem and do not need treatment; others need surgery, sometimes even before the child has turned one year old. Cardiologists (heart specialists) often classify congenital heart disease into cyanotic and acyanotic types. Cyanotic means that the heart problem is causing too little blood to pass through the lungs. As a result, the baby’s blood is not carrying enough oxygen, and the baby may become cyanotic (look bluish). In acyanotic heart disease, the heart problem causes too much blood to pass through the lungs, resulting in increased pressure and stress on the baby’s lungs. Here is a summary of some of the various kinds of congenital heart disease (AHA, 2018):
Signs and symptoms of congenital heart disease
Signs and symptoms of congenital heart disease vary depending on the type, severity, and number of heart defects. You may see signs right after birth, within the first year, or even in adulthood. Some babies have no symptoms at all. When symptoms do occur, they may include:
Blue-tinted skin, nails, or lips (cyanosis)
Rapid or difficulty breathing
Fatigue, especially when feeding
Sleepiness
Poor weight gain
Heart murmurs
Poor circulation
Causes of congenital heart disease
In congenital heart disease, the baby’s heart does not develop normally before birth. The exact causes of CHD are not well understood, but several factors may play a role. Genetics may play a role in some types; according to the American Heart Association (AHA), there is a 2–15% risk of congenital heart disease running in the family (AHA, n.d.). Most likely, it is a combination of genetic and environmental factors. Researchers believe that a mother’s exposure to specific environmental factors, like cigarette smoke or certain medications (ACE-inhibitors and retinoic acids), can increase the risk of her child have congenital heart disease (NIH, n.d.). Medical conditions like diabetes, phenylketonuria, and rubella infections in the mother may also make congenital heart disease more likely (NIH, n.d.). It is important to know that, in most cases, there is no identifiable cause.
Diagnosis of congenital heart disease
Some congenital heart defects can be diagnosed before the baby is born by doing an ultrasound. Others are diagnosed after birth or even in adulthood. Your child’s pediatrician will perform a physical exam and evaluate at the baby’s appearance, listen to the heart and lungs, and look for any signs of difficult or rapid breathing, growth delays, or bluish skin. If necessary, additional testing may be needed, including:
Electrocardiogram (EKG or ECG): test to look at the rhythm of the heart
Echocardiogram: an ultrasound of the heart that can diagnose structural problems
Chest X-ray: can determine if the heart is too large
Cardiac MRI: give detailed imaging of the heart
Treatment of congenital heart disease
Treatment and the timing of the intervention depend on the type of heart disease and its symptoms. Some forms of CHD do not require any treatment, while critical congenital heart disease will need surgery within the first year of life. Others may need treatments throughout their lives. The main types of treatment are medications, cardiac catheterization, and surgery.
Medication: Prescribing ibuprofen or acetaminophen may help a patent ductus arteriosus close.
Cardiac catheterization: This is sometimes useful for repairing simple heart defects, like atrial septal defects, patent ductus arteriosus, or narrowing of valves or arteries. During this procedure, a thin tube is inserted into a vein in your groin, arm, or neck, and guided into your heart.
Cardiac surgery: This may be required to treat congenital heart disease. It might be needed to close a hole in the heart, to repair a complex defect, to repair or replace a valve, or to widen narrow blood vessels. The type of surgery performed depends on the heart problem and can include a heart transplant, temporary surgery, implantable heart device (i.e. implantable cardioverter defibrillators), or other kinds of open-heart surgery.
How to prevent congenital heart disease
Even though most cases come from unknown causes, mothers can decrease the risk that their children will have congenital heart disease by taking the following actions:
Avoid smoking or exposure to secondhand smoke while pregnant.
Talk to your healthcare provider about any medications (prescription or over-the-counter) that you are taking to make sure they are safe for pregnancy.
Make sure you have your diabetes and phenylketonuria under control before and throughout pregnancy.
If you were never vaccinated against rubella, talk to your healthcare provider about how to avoid exposure to it.
If congenital heart disease runs in your family, talk to your healthcare provider about your child’s risk of heart defects; you may want to consider genetic counseling.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
American Heart Association (AHA). (8 May, 2018). About Congenital Heart Defects. Retrieved on Feb. 7, 2020 from https://www.heart.org/en/health-topics/congenital-heart-defects/about-congenital-heart-defects
American Heart Association (AHA). (n.d.). Understanding Your Risks for Congenital Heart Defects. Retrieved on Feb. 7, 2020 from https://www.heart.org/en/health-topics/congenital-heart-defects/understand-your-risk-for-congenital-heart-defects
Centers for Disease Control and Prevention (CDC). (12 November, 2019). What are Congenital Heart Defects? Retrieved on Feb. 7, 2020 from https://www.cdc.gov/ncbddd/heartdefects/index.html
National Institutes of Health (NIH). (n.d.). National Heart, Lung, and Blood Institute - Congenital Heart Defects. Retrieved on Feb. 7, 2020 from https://www.nhlbi.nih.gov/health/congenital-heart-defects










