Diabetes: causes, symptoms, diagnosis, and treatment

Reviewed by Melynda Barnes, MD, Ro,
Written by Tzvi Doron, DO
last updated: May 14, 2019
11 min read
Here's what we'll cover
Diabetes mellitus is a chronic disease that causes blood glucose to become higher than normal. Glucose is the fuel the body uses to perform all of its functions. When blood glucose rises to abnormal levels, it is called hyperglycemia. The word “diabetes” means to siphon in Greek. It was noticed that people with diabetes passed large amounts of urine. “Mellitus” is Latin for sweet because it was also noted that the urine of people with diabetes tasted sweet due to the high amount of sugar it contained.
There are two types of diabetes mellitus. In type 1 diabetes, the body’s immune system destroys the cells in the pancreas that produce insulin. Insulin is the hormone that regulates the use of glucose in the body. In type 2 diabetes, the body’s cells do not respond normally to insulin (called insulin resistance). The CDC estimates that almost 10% of Americans have diabetes (CDC, 2017), including around 30 million adults. Approximately 1 in 4 people don’t even know they have diabetes.
Diabetes is the seventh leading cause of death in the US and one of the most costly diseases with estimated costs of $327 billion in 2017 (Diabetes Care, 2017). The good news is that the modern treatment of diabetes is evolving. And with some knowledge about diabetes treatment and prevention, you can take steps to improve your health and live your best life.
Weight loss
Get access to GLP-1 medication (if prescribed) and 1:1 support to meet your weight goals
It’s all about insulin
Diabetes is a disease of disordered insulin physiology, meaning that insulin’s function in the body is abnormal (Wilcox, 2005). This can be due to not making enough insulin (type 1), or the cells of the body being resistant to the effects of insulin (type 2). So what is insulin, and what does it do?
Insulin is a peptide hormone, which means it is made out of protein. Hormones are molecules that are made by glands and released into the bloodstream where they travel to other organs and carry messages to them. Peptide hormones work by binding to receptors on cell membranes and sending messages into the cell from there. There is also another type of hormone, called steroid hormones, that are made out of cholesterol. Steroid hormones work by crossing cell membranes and delivering their messages to the cell more directly.
Insulin has many functions in the body. One of its main functions is to regulate the amount of glucose in the blood. Insulin’s control of blood sugar can be summarized in the following steps:
When you eat a meal containing carbohydrates or proteins, the pancreas is signaled to release insulin into the bloodstream.
Many cells in the body contain insulin receptors on their surfaces. When insulin binds to its receptors, a chain reaction takes place that allows glucose to enter muscle and fat cells.
Insulin also signals the liver to stop making glucose (a process called gluconeogenesis) and start making glycogen, which is a storage form of glucose.
Taken together, these actions prevent blood sugar levels from shooting through the roof after eating a meal. Soon after being eaten, food is broken down into its components—and glucose is one of those components. Regulating glucose levels is vital to keep the body running properly. When people don’t make enough insulin (type 1 diabetes) or their cells are not responsive to insulin (type 2 diabetes), blood sugar levels rise (hyperglycemia). Now you can see why insulin is so important when we talk about diabetes.
Types of diabetes
The three most important types of diabetes are type 1, type 2, and gestational diabetes. All three result in higher blood sugar levels, but they are different and require different treatment.
Type 1 diabetes basics
Type 1 diabetes is an autoimmune disease, which means the body’s own immune system destroys the cells in the pancreas that produce insulin. This usually happens in childhood or early adulthood. Without insulin, glucose (sugar) can’t get into the cells. This causes death within a few weeks, and until the 1920s type 1 diabetes was always fatal. In the early 1920s, Eli Lilly started to mass-produce insulin from pigs’ and cows’ pancreases (Wilcox, 2005). This was the first treatment for type 1 diabetes and did prolong people’s lives. The problem with insulin taken from animals is that it is slightly different from human insulin. This caused people to start producing antibodies to it and to have allergic reactions.
Over the next several decades, scientists figured out how to make human insulin through genetic engineering, as well as how to make longer and shorter-acting insulins. These advancements solved the problem of allergic reactions, but also helped prevent or delay complications of diabetes, such as blindness and kidney damage. Today, there are at least five types of insulin with different lengths of action that are sold by many pharmaceutical companies. This allows for treatment to be tailored to the individual.
Type 1 diabetes treatment always requires insulin injections. Treating risk factors for cardiovascular disease is also an important part of treatment since type 1 diabetes is itself a risk factor for cardiovascular disease. This includes treating high blood pressure and cholesterol levels, being physically active, and quitting smoking.
Type 1 diabetes risk factors and causes
The exact cause of type 1 diabetes is not known, but a combination of genetic and environmental factors are at play. Specific genes people inherit from their parents predispose them to diabetes, but an environmental trigger is necessary to cause diabetes. Scientists think that certain viruses can trigger the immune system to attack and destroy the cells in the pancreas that produce insulin. Risk factors for type 1 diabetes include:
Family history: Having a parent or sibling with type 1 diabetes increases the risk of developing diabetes.
Age: Type 1 diabetes has two age peaks, one between ages 5 and 7 and another around puberty, although it can occur later in life, too.
Race: Caucasians have a higher risk of type 1 diabetes than other ethnicities (CDC, 2019).
Type 2 diabetes basics
In type 2 diabetes, the pancreas produces enough insulin (in the early stages), but the body’s cells do not respond to it as they should. Over time, the body produces more and more insulin to overcome the cells’ resistance to its effects. Eventually, the pancreas itself becomes damaged and cannot produce enough insulin.
Since the cells’ resistance causes type 2 diabetes to insulin, the treatment is different than for type 1 diabetes. The backbone of treatment is lifestyle modification, including weight loss, exercise, and a healthy diet. There are also at least eight classes of drugs used to treat type 2 diabetes. These drugs work through different mechanisms. Some of them increase the body’s production of insulin to overcome insulin resistance. Others work by lowering the liver’s production of sugar, while some work by increasing the amount of sugar that leaves the body in the urine. Insulin is also used in type 2 diabetes when the disease advances. Like type 1 diabetes, type 2 diabetes is a major risk factor for heart attack and stroke, so part of the treatment is aggressive management of cardiovascular risk factors. This includes treating high blood pressure and cholesterol levels and quitting smoking.
Type 2 diabetes risk factors and causes
Type 2 diabetes is caused by a mixture of genetic, environmental, and lifestyle factors. The most important risk factors for type 2 diabetes are:
Being overweight or obese: According to the World Health Organization (WHO), 90% of people with type 2 diabetes are overweight or obese (WHO, 2003).
Age: The risk of type 2 diabetes increases after the age of 45.
Sedentary lifestyle: Living an active lifestyle is protective against type 2 diabetes.
Race: Certain ethnicities have a higher risk of type 2 diabetes. These include African Americans, Native Americans and Native Alaskans, Hispanics, and Pacific Islanders.
Women who have had gestational diabetes
Women with polycystic ovary syndrome (PCOS)
People with prediabetes
People with high blood pressure
Gestational diabetes basics
Gestational diabetes occurs in pregnant women who did not have diabetes before pregnancy. This increases the risks of developing preeclampsia and incubating babies who are too big to deliver vaginally. The cause of gestational diabetes is not fully understood. Pregnancy itself produces a state of insulin resistance (Plows, 2018). In people with background insulin resistance, this can cause blood sugar levels to rise to the point of having diabetes. The cornerstone of gestational diabetes treatment is diet modification. These changes aren’t enough for some women who will need to take insulin or oral medication (e.g., metformin) to control their blood sugar. It’s important to note that women who get gestational diabetes are at higher risk for developing type 2 diabetes later in life.
Gestational diabetes risk factors and causes
Many of the risk factors for gestational diabetes are the same as for type 2 diabetes, including:
Being overweight or obese
Being over 35
Having a sedentary lifestyle
Ethnic background. Certain ethnicities have a higher risk of gestational type 2 diabetes. These include African Americans, Native Americans and Native Alaskans, Hispanics, and Pacific Islanders.
Women who have had gestational diabetes with a previous pregnancy or have given birth to a baby weighing more than 9 lbs
Women with polycystic ovary syndrome (PCOS)
Women with prediabetes prior to pregnancy
Women with high blood pressure or a history of heart disease
Prediabetes: a crossroads
Prediabetes is a condition that precedes type 2 diabetes. In prediabetes, the body already has trouble regulating blood sugar, but levels aren’t quite in the diabetic range yet. People with prediabetes don’t automatically develop type 2 diabetes. Lifestyle changes like weight loss and exercise can prevent the progression from prediabetes to diabetes (Diabetes Prevention Program Research Group, 2002). Metformin, a medication used to treat type 2 diabetes, can also prevent the progression of prediabetes to type 2 diabetes in some people.
Symptoms of diabetes
The symptoms of diabetes are related to high levels of blood sugar. The classic symptoms of type 1 diabetes include:
Urinating more than usual (including at night)
Extreme thirst and hunger
Weight loss despite eating a lot
Weakness and fatigue
Symptoms of advanced type 2 diabetes and gestational diabetes are similar to type 1 diabetes. However, it’s important to understand that people with type 2 diabetes and gestational diabetes often don’t have symptoms unless the disease is advanced, and their blood sugar is extremely high. That’s why regular diabetes screening is essential.
Having blood sugar that is very high for long periods increases the risks of damage to organs, including the eyes, kidneys, and nerves. When these organs sustain damage, people can experience serious symptoms like blindness, nerve pain, and signs and symptoms of kidney failure (difficulty breathing, fatigue, itching, anemia, bone fractures, etc.).
Diagnosing types 1 & 2 diabetes and prediabetes
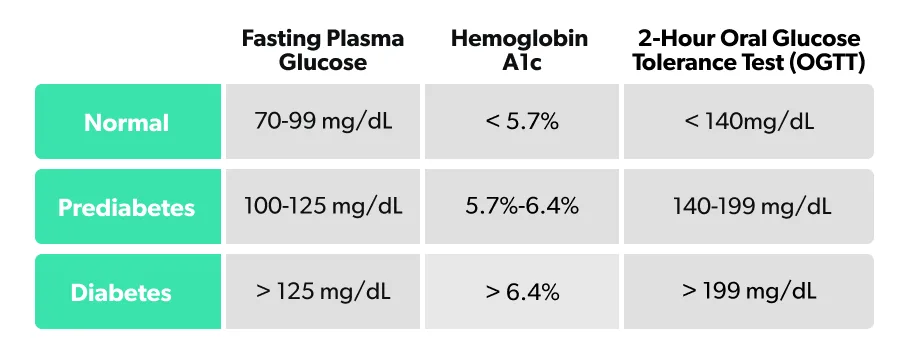
Doctors typically use one of three tests to diagnose diabetes or prediabetes:
Fasting plasma glucose: You fast for eight hours (no food or drinks, only water), then measure your blood sugar levels.
Hemoglobin A1C: Sometimes called glycated hemoglobin, this is an overall measure of how many hemoglobin particles in your blood are stuck to sugar molecules.
2-hour Oral Glucose Tolerance Test (OGTT): Involves drinking 75 g (about 2 ½ ounces) of glucose (sugar) then measuring your blood sugar (and sometimes insulin levels) two hours later.
Your body is always processing glucose and using it for energy. That means your glucose levels can fluctuate throughout the day or after certain activities like eating, sleeping, or exercise. This constant flux makes accurately measuring glucose levels tricky. That’s why, under most circumstances, doctors require a confirmatory test if one of these tests is abnormal before making a diagnosis.
Each glucose test has its pros and cons, and your doctor may prefer one test over another, depending on the person. For instance, the OGTT test is rarely done, outside of diagnosing pregnant women for gestational diabetes. In comparison, the Hemoglobin A1C test has the advantage of not being affected if you eat right before the test. Fasting glucose and Hemoglobin A1C are often used together as they can be included in the same blood draw after an overnight fast.
How to read your glucose test
Your glucose test result ranges should fall in one of three categories: Normal, Prediabetic, and Diabetic. In case these sections aren’t highlighted, here are the glucose ranges for normal, prediabetes, and diabetes in each test:
Diagnosing gestational diabetes
The American Diabetes Association (ADA) recommends that all pregnant women be screened for gestational diabetes at 24–28 weeks regardless of their history (ADA, 2017). There are two methods for screening for gestational diabetes, the one-step method and the two-step method. The one-step method involves drinking 75 g of glucose and then measuring blood glucose one and two hours later. The-two step method involves drinking 50 g of glucose and then measuring blood glucose one hour later. If the one-hour glucose is above 130, the second step is performed with a 100 g glucose drink. The cutoffs for diagnosing gestational diabetes for the one-step method and step two of the two-step method are:
Fasting glucose: one-step >91 mg/dL; two-step > 95 mg/dL
One hour glucose: >180 mg/dL for both tests
Two hour glucose: one-step >153 mg/dL; two-step > 155 mg/dL
Three hour glucose: one-step > not measured; two-step >140 mg/dL
Sugar in my urine?
Rarely, other tests are used for various purposes in people with diabetes. Under normal circumstances, the kidney filters glucose into the urine during the process of filtering the blood. However, there is normally no glucose found in the urine because the kidney has special transporters that reabsorb the glucose into the blood.
When glucose levels in people with diabetes get above 200–250 mg/dL, these transporters reach max capacity and glucose starts to spill into the urine (Osaki, 2016). In these cases, a urine dipstick will find glucose. Incidentally, many of the symptoms of high blood sugar occur because of this. Glucose in the urine causes there to be higher volumes of urine. When people with very high sugar levels urinate too much, they become dehydrated. This results in weight loss, fatigue, weakness, and extreme thirst. A secondary cause of weight loss can involve the loss of calories from the glucose getting lost in the urine.
What about ketones?
For the most part, diabetes is a chronic, treatable disease these days, but diabetic emergencies still happen. One of the most important diabetic emergencies is called diabetic ketoacidosis (DKA). It is much more common with type 1 diabetes than it is in type 2 diabetes. DKA occurs due to an extreme deficiency of insulin. It can also be caused by higher than normal insulin requirements due to stress, such as from trauma, infections, and heart attacks. Usually, people with DKA have very high glucose levels (over 250 mg/dL). In rare cases, people do not have these very high glucose levels. It’s a complicated process, but the basics are as follows.
An extreme deficiency of insulin causes glucose to be unable to enter cells.
The cells start to burn amino acids and fatty acids for energy because they do not have access to glucose.
Burning very large amounts of fatty acids results in some fatty acids being metabolized incompletely.
This partial burning of fatty acids produces large amounts of two ketones, called beta-hydroxybutyrate and acetoacetate. These ketones are acidic and make the blood acidic.
Very high levels of blood sugar cause the person to urinate large amounts of urine, causing severe dehydration.
Large amounts of potassium are lost in the urine, causing depletion of the body’s potassium.
The signs and symptoms of DKA include:
Nausea and vomiting
Abdominal pain
Lethargy and fatigue
Fast heart rate (tachycardia)
Rapid, deep breaths (Kussmaul breathing)
Fruity smell to the breath
In severe cases, confusion can be caused by swelling to the brain.
DKA is a medical emergency and can result in death in up to 5% of cases (BMJ, 2015). The diagnosis of diabetic ketoacidosis is based on having an acidic blood pH (<7.3), elevated ketone levels in the blood and/or urine, and glucose levels, along with other labs measuring kidney function electrolytes in the blood.
Treatment of DKA includes large amounts of IV fluid, IV insulin, and mineral replacement to correct the mineral deficiencies. Education is important to prevent recurrence.
Living with diabetes
Living with diabetes can be challenging. It can cause anxiety around food choices, and food should be one of life’s great pleasures. Type 1 diabetes and gestational diabetes can be particularly challenging as they require multiple daily blood sugar checks traditionally done by finger prick. Some people with type 2 diabetes (those who use certain medications, including insulin) need to do this, too. And then there are all the concerns about long-term health. Will I have a heart attack in my 40s? Will I be able to see my children graduate college or play with my grandchildren? Will diabetes prevent me from accomplishing my career goals? These are just some of the questions people may ask about how diabetes will affect their lives.
The good news is that there has never been more available to help people with diabetes live the best lives possible. Medical advances in diabetes management and risk factor reduction of diabetes complications are an important part of the story.
The last few years have seen new medications that decrease cardiovascular risk in patients with type 2 diabetes. Some of these medications can also help with weight loss. Bariatric surgery has become much safer than it was in its early days, and in some cases can cause remission of diabetes.
Exciting things in development include the bionic pancreas and islet cell transplants. This entails transplanting healthy insulin-producing cells to a person with type 1 diabetes so that they can make their own insulin.
Besides medical advances, there are many other resources available today to help people manage their diabetes. Today, apps can help with better food choices. Insulin pumps and continuous glucose meters (CGMs) can help people with type 1 diabetes manage their insulin regimens. Support groups and diabetes educators can help educate people on how to take care of their diabetes while still living life to its fullest.
With the right education and support, people with diabetes can live fulfilling lives, and with modern medicine, they can live longer and healthier lives.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
American Diabetes Association. (2017). 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2018. Diabetes Care , 41 (Supplement 1). doi: 10.2337/dc18-S002. Retrieved from https://care.diabetesjournals.org/content/41/Supplement_1/S13
Centers for Disease Control and Prevention. (n.d.). National Diabetes Statistics Report, 2017 . National Diabetes Statistics Report, 2017 . U.S. Dept of Health and Human Services. Retrieved from https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf
Centers for Disease Control and Prevention. (August 28, 2019). Who's at Risk? Retrieved from https://www.cdc.gov/diabetes/basics/risk-factors.html
Diabetes Prevention Program Research Group. (2002). Reduction in the Incidence of Type 2 Diabetes with Lifestyle Intervention or Metformin. New England Journal of Medicine , 346 (6), 393–403. doi: 10.1056/nejmoa012512. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMoa012512
Diabetic ketoacidosis in adults. (2015). BMJ . doi: 10.1136/bmj.h5866. Retrieved from https://www.bmj.com/content/351/bmj.h5866
Economic Costs of Diabetes in the U.S. in 2017. (2018). Diabetes Care , 41 (5), 917–928. doi: 10.2337/dci18-0007. Retrieved from https://care.diabetesjournals.org/content/41/5/917
Osaki, A., Okada, S., Saito, T., Yamada, E., Ono, K., Niijima, Y., Hoshi, H., & Yamada, M. (2016). Renal threshold for glucose reabsorption predicts diabetes improvement by sodium-glucose cotransporter 2 inhibitor therapy. Journal of Diabetes Investigation , 7 (5), 751–754. doi: 10.1111/jdi.12473. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/27181936
Plows, J., Stanley, J., Baker, P., Reynolds, C., & Vickers, M. (2018). The Pathophysiology of Gestational Diabetes Mellitus. International Journal of Molecular Sciences , 19 (11), 3342. doi: 10.3390/ijms19113342. Retrieved from https://www.mdpi.com/1422-0067/19/11/3342
Wilcox, G. (2005). Insulin and Insulin Resistance. The Clinical Biochemist Reviews . Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1204764/
World Health Organization. (2003). Obesity and Overweight . Obesity and Overweight . Retrieved from https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight









