What to expect during a prostate exam

Reviewed by Tzvi Doron, DO,
Written by Chimene Richa, MD
last updated: May 05, 2021
5 min read
Here's what we'll cover
If your healthcare provider has recommended you get your first prostate exam, you might feel a bit nervous, but don’t worry! While it may not be the most comfortable test, it’s certainly not painful, and the whole test takes just a few minutes.
Let’s go over what to expect during a prostate exam, who should get tested, and the risks and benefits.
What is a prostate exam?
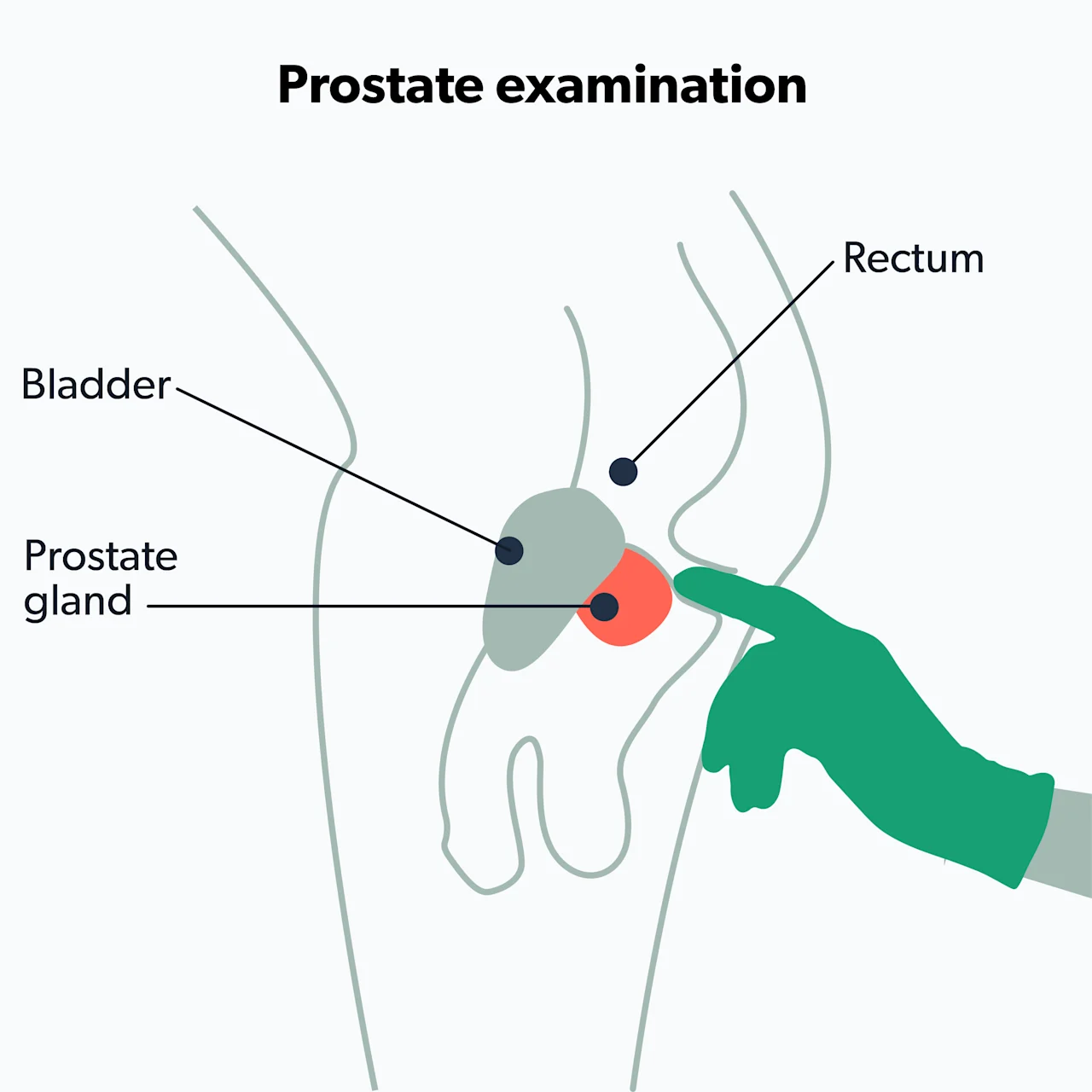
The prostate exam, or digital rectal exam (DRE), allows your healthcare provider to check on the health of your prostate gland. Some providers have used it as an element of prostate cancer screening.
After reviewing several studies, experts now recommend against using the prostate exam in prostate cancer screening because the DRE may not be effective for prostate cancer screening. However, many healthcare providers still use it for other purposes or combined with the PSA test for prostate cancer screening (Naji, 2018).
The prostate gland sits just in front of the rectum. Your healthcare provider can reach it by gently inserting a finger in the rectum via the anus. They'll manually feel your prostate to look for larger than usual areas, lumps, hard spots, tenderness, or any other problems. While performing the DRE, the healthcare provider can also check for other issues in or around the rectum, like hemorrhoids, anal fissures, blood in the stool, etc.
Who should get a prostate exam?
One of the big questions that experts have examined over the years is when men should get a prostate exam. According to the American Urological Association (AUA), if you are over the age of 50 and have an average risk of developing prostate cancer, you should talk to your healthcare provider about the risk and benefits of a prostate exam (Carter, 2013).
However, suppose you are at a higher risk of prostate cancer or are experiencing urinary or sexual symptoms. In that case, you should have a discussion with your healthcare provider about prostate cancer screening sooner rather than later. People who may have a high risk of prostate cancer include (Carter, 2013):
African Americans
Men with a family history of prostate cancer or who have tested positive for BRCA1, BRCA2, or HOXB13 gene mutations
Men with symptoms like blood in the urine, painful or frequent urination, or sexual problems—these may be signs of problems with the prostate, including prostate cancer.
What happens during a prostate exam
If you’ve never had a DRE before, you may be concerned about what happens during a prostate exam and what it feels like. Don’t worry—it is not a painful experience.
Before performing a prostate exam, your healthcare provider will ask you to remove your clothes from the waist down and will provide you with a gown to wear. During the DRE, you will stand and bend at the waist or lie on your side with your knees bent. Your healthcare provider will apply lubricant to a gloved finger, gently insert it into your rectum, and sweep their finger along the wall of the rectum—this allows them to feel any abnormalities in the prostate.
Your provider may press down on your lower abdomen during this process, potentially causing mild discomfort and the urge to urinate—this is normal. The good news is these sensations only last a few minutes.
Things to do before a prostate exam
You don’t have to do anything special to prepare for a prostate exam. You may get one as part of your annual checkup or during an appointment to discuss a specific issue.
Prostate-specific antigen (PSA) test
Along with the DRE, many healthcare providers will also order a test for prostate-specific antigen (PSA), a protein produced by the prostate. The PSA blood test has become the mainstay of prostate cancer screening as it's far more sensitive than the DRE at picking up cancers.
While measuring PSA levels is important in prostate cancer screening, an abnormal PSA test does not necessarily mean that you have prostate cancer. A PSA outside of the normal range could be due to an enlarged prostate, prostatitis, a urinary tract infection (UTI), among other reasons. Your healthcare provider will help you interpret PSA test results and recommend further testing if necessary.
Various organizations have slightly different recommendations regarding screening. This table illustrates the American Urological Association (AUA) recommendations for prostate cancer screening (Carter, 2013).
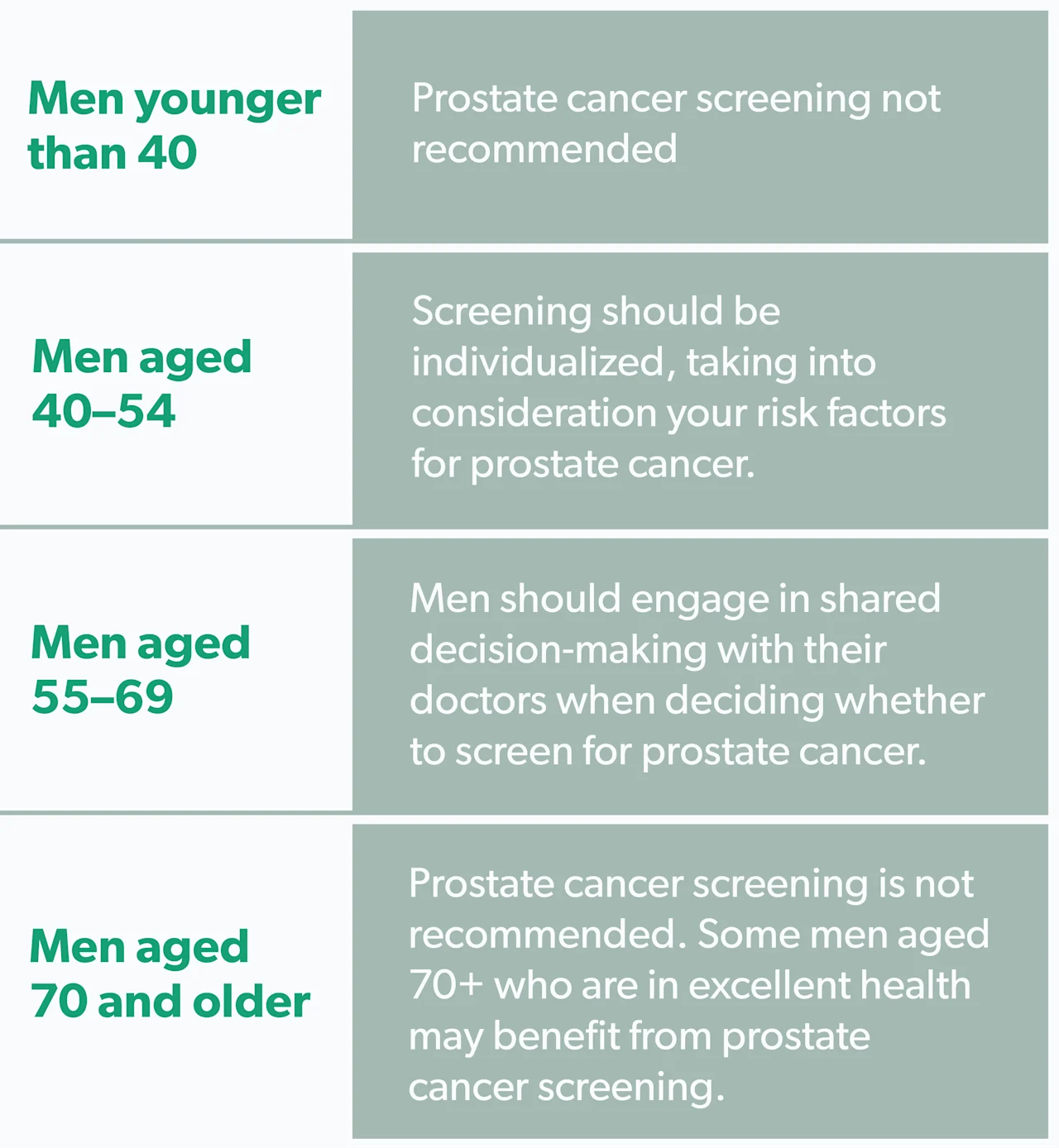
The United States Preventive Services Task Force (USPSTF) has very similar recommendations to the AUA. However, they do not comment on men under age 55 or 70+ in excellent health (USPSTF, 2018).
Results and follow up
After a DRE, your healthcare provider will know right away if there are any problems like lumps or a prostate that is larger than usual (as in benign prostatic hyperplasia, or BPH). You will discuss any findings with your provider and plan the next steps. The results from a PSA test typically take around two weeks to come back, and your healthcare provider will go over these with you.
If all of your test results are normal, and you and your provider decide to continue screening, you will most likely need testing every two years. However, if the PSA test is abnormal, your healthcare provider may refer you to a urologist for additional testing.
Risks and benefits of prostate cancer screening
There are two main benefits of prostate cancer screening.
One is potentially preventing death from prostate cancer. Many men have prostate cancer without experiencing symptoms, so screening can potentially identify prostate cancer early on when it can be treated more easily.
Another benefit of screening and early detection is potentially catching prostate cancer in its early stages, allowing for more effective treatment. Earlier treatment can help prevent prostate cancer from spreading beyond the prostate (metastatic prostate cancer), which can cause several symptoms.
Unfortunately, there are drawbacks to prostate cancer screening. The DRE is not very sensitive or specific. This means that people who have prostate cancer can still have a normal DRE, while patients with an abnormal DRE may not have prostate cancer. For these reasons, healthcare providers are no longer performing DRE alone for routine prostate cancer screening and relying instead on the PSA test (Naji, 2018).
PSA testing also has limitations in screening for prostate cancer. Elevated PSA levels do not only occur in prostate cancer. Prostatitis (inflammation of the prostate) or an enlarged prostate (BPH) can also cause PSA levels outside the normal range. Abnormal test results can ultimately lead to undue anxiety and further testing that may prove unnecessary (Hoffman, 2021).
Another problem with the PSA test is the potential for overdiagnosis and overtreatment. Screening uncovers patients with prostate cancer who would otherwise never have had any issues resulting from the disease.
This overdetection means that PSA testing leads to more men getting prostate cancer diagnoses. Once someone is diagnosed, he may elect to undergo prostate cancer treatment, which is not without risks. Treatment risks include infections, bleeding, and urinary problems due to biopsies. Treatment can also cause erectile dysfunction (ED), urinary incontinence, and fecal incontinence (Hoffman, 2021).
Overall recommendations
Routine prostate cancer screening, especially for men younger than 40, is not recommended. The prostate exam is no longer used for routine prostate cancer screening, though it is sometimes still used in conjunction with a PSA test. Screening tests have their own risks and benefits. The most significant risk is overtreatment, a direct result of overdiagnosis.
Current prostate exam screening recommendations vary based on your age, risk factors, and any symptoms you may or may not be experiencing. There is no "one-size-fits-all" for prostate exams and cancer screenings. Discuss your risk of prostate cancer with your healthcare provider. Together, you can decide whether to screen for prostate cancer and the best screening plan for you.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
American Cancer Society (ACS). (2021). American Cancer Society recommendations for prostate cancer early detection. Retrieved on May 3, 2021 from https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging/acs-recommendations.html
Carter, H. B., Albertsen, P. C., Barry, M. J., Etzioni, R., Freedland, S. J., et al. (2013). Early detection of prostate cancer: AUA Guideline. The Journal of Urology, 190 (2), 419–426. doi: 10.1016/j.juro.2013.04.119. Retrieved from https://pubmed.ncbi.nlm.nih.gov/23659877/
Hoffman, R.M. (2021). Screening for prostate cancer. In UptoDate . Elmore, J.G., O’Leary, M.P, and Givens, J. (Eds.). Retrieved from https://www.uptodate.com/contents/screening-for-prostate-cancer
Naji, L., Randhawa, H., Sohani, Z., Dennis, B., Lautenbach, D., Kavanagh, O., et al. (2018). Digital rectal examination for prostate cancer screening in primary care: a systematic review and meta-analysis. The Annals of Family Medicine, 16 (2), 149–154. doi: 10.1370/afm.2205. Retrieved from https://pubmed.ncbi.nlm.nih.gov/29531107/
US Preventive Services Task Force (USPSTF), Grossman, D. C., Curry, S. J., Owens, D. K., Bibbins-Domingo, K., Caughey, A. B., et al. (2018). Screening for prostate cancer: US Preventive Services Task Force recommendation statement. JAMA, 319 (18), 1901–1913. doi: 10.1001/jama.2018.3710. Retrieved from https://pubmed.ncbi.nlm.nih.gov/29801017/










