Prostate massage: health benefits of hitting the male G-spot
Written by Michael Martin and
Written by Michael Martin and
last updated: Jun 17, 2022
4 min read
Here's what we'll cover
Sometimes referred to as the male G-spot, the prostate gland is a reproductive organ that can get inflamed and grow enlarged as you age. If you deal with an enlarged prostate, prostate pain, or have a chronic health condition, treatments like prostate massage may help.
What is a prostate massage?
Prostate massage is a technique used to alleviate symptoms of an enlarged or inflamed prostate. It’s also being explored for use in medical settings to treat certain health conditions, although more research is needed.
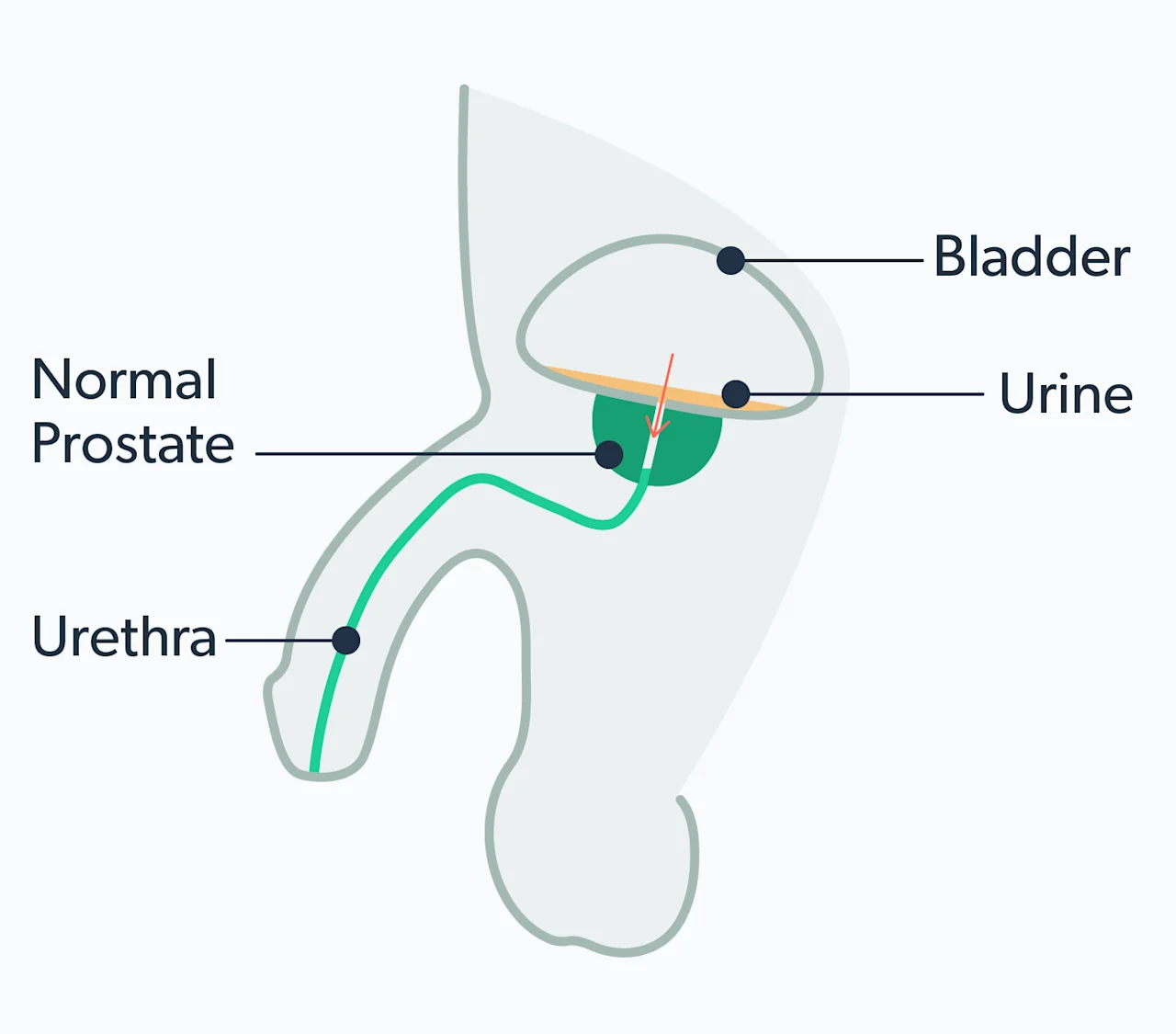
A prostate massage involves inserting a finger into the rectum to stimulate the prostate gland. This roughly walnut-sized gland sits between the bladder and penis just in front of the rectum. The prostate’s main function is producing semen, a fluid that nourishes sperm and helps it travel.
Massaging the prostate encourages the prostate ducts to empty seminal fluid, which may have certain health benefits. Prostate massages can also be performed for sexual stimulation, resulting in a prostate orgasm (hence the name, male G-spot).
Prostate milking vs. massage: what’s the difference?
You may have heard the term “milking” used to describe a prostate massage. While similar, prostate milking refers more to stimulating the prostate for sexual pleasure. It also means (as the name implies) massaging until a fluid or pre-ejaculate is released.
Health benefits of prostate massage
As men age, the prostate can become enlarged. Certain conditions can also agitate or enlarge the prostate, causing uncomfortable symptoms like difficulty urinating and frequently feeling like you have to pee. Research is limited, but studies suggest prostate massage may relieve these symptoms and help treat certain health conditions.
Regular ejaculation is said to have a host of physical and mental benefits, including a reduced risk of heart disease and prostate cancer. One way to ejaculate regularly is through prostate massage, with a partner or on your own.
What conditions can prostate massage help treat?
Much of the current research on prostate massage therapy is limited or inconclusive. That said, some men experience health benefits or symptom relief from regular prostate massage.
Here are some of the medical conditions a prostate massage might benefit.
Benign prostatic hyperplasia (BPH)
BPH is a type of prostate enlargement that is non-cancerous. It’s common with age, primarily affecting people over 50 (Lokeshwar, 2019).
Like other prostate conditions, BPH causes urinary tract symptoms like loss of bladder control (incontinence) and difficulty fully emptying the bladder. Limited studies have found therapeutic prostate massage may show promise in alleviating BPH symptoms (Capodice, 2009).
Chronic prostatitis
Inflammation of the prostate due to infection or injury can lead to prostatitis, a disease characterized by pain and difficulty urinating. People with this condition often experience difficulty urinating, pain in the pelvic area, and flu-like symptoms.
The data is inconclusive regarding whether prostate massage helps with chronic prostatitis. Several studies suggest it can help improve symptoms, while others find the technique ineffective (Franco, 2018).
The consensus? Prostate massage isn’t a magic bullet for prostatitis but may provide relief. However, prostate massage is not part of the standard treatment for enlarged prostate or prostatitis.
Prostate cancer
While scientists can’t credit prostate massage directly, several studies show there may be health benefits to regular ejaculation, including a lower risk of prostate cancer. Aside from lung cancer, prostate cancer is the most common cancer in men (Rawla, 2019).
A long-term study by Harvard Medical School found that men who reported ejaculating 21 or more times a month had a lower risk of prostate cancer than those who ejaculated 4–7 times a month (Rider, 2016).
That said, the jury is still out on whether frequent ejaculation reduces someone’s risk for prostate cancer. Prostate cancer also has its own considerations, treatments, and therapies, and massaging the prostate is not a recommended treatment.
What to expect during a prostate massage
When getting a prostate massage, the one conducting it inserts a gloved and lubricated finger into the rectum. From there, they will slowly press or rub the prostate. This may feel awkward or uncomfortable, but it shouldn’t be painful.
The intent is to relieve pressure or reduce swelling by releasing built-up fluid in the prostate. The massage doesn’t last too long and can be done several times a month to relieve symptoms.
How to massage the prostate
The prostate has gotten a lot of press for being an underrated source of sexual pleasure for men, similar to the G-spot in women. Studies also suggest that prostate-induced orgasms may produce more intense and satisfying stimulation than penile stimulation (Levin, 2018).
If you’re investigating prostate play for pleasure, here’s how to do it:
Apply lube around the anus and the finger you’re using.
Gently insert a finger and feel for a round lump a few inches inside the rectum. You may need to re-apply lube several times throughout.
Press or massage the gland with the pad of your finger. Keep going for as long as you or your partner wishes––or until orgasm is achieved.
There are many ways to do a prostate massage, including with a partner, by yourself, or with a prostate massage toy. You can also perform an external prostate massage by rubbing or putting pressure on the perineum, the spot roughly halfway between the scrotum and anus.

Prostate massage risks
Prostate massage is natural and shouldn’t pose many safety risks. A common side effect is soreness. If you’re performing a self prostate massage, pressing too hard could cause pain or injury to the area.
You should avoid prostate massages if you have hemorrhoids or bacterial prostatitis, as it could cause inflammation or bacteria to spread. If you’re trying an electronic prostate massage, make sure you know how to use it properly or ask a medical professional for instructions.
DISCLAIMER
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
Ateya, A., Fayez, A., Hani, R., et al. (2006). Evaluation of prostatic massage in treatment of chronic prostatitis. Urology , 67 (4), 674–678. doi:10.1016/j.urology.2005.10.021. Retrieved from https://www.aafp.org/pubs/afp/issues/2010/0815/p397.html
Capodice, J. L., Stone, B. A., & Katz, A. E. (2009). Evaluation of an at-home-use prostate massage device for men with lower urinary tract symptoms. The Open Urology & Nephrology Journal , 2 , 20–23. doi:10.2174/1874303X01002010020. Retrieved from https://openurologyandnephrologyjournal.com/VOLUME/2/PAGE/20/FULLTEXT/
Franco, J. V., Turk, T., Jung, J. H., et al. (2018). Non-pharmacological interventions for treating chronic prostatitis/chronic pelvic pain syndrome. T he Cochrane Database of Systematic Reviews, 5 (5), CD012551. doi:10.1002/14651858.CD012551.pub3. Retrieved from https://pubmed.ncbi.nlm.nih.gov/29757454/
Hennenfent, B., Lazarte, A., & Feliciano, A. (2006). Repetitive prostatic massage and drug therapy as an alternative to transurethral resection of the prostate. Medscape General Medicine , 8 (4), 19. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1868377/
Levin, R. J. (2018). Prostate-induced orgasms: A concise review illustrated with a highly relevant case study. Clinical Anatomy , 31 (1), 81–85. doi:10.1002/ca.23006. Retrieved from https://onlinelibrary.wiley.com/doi/full/10.1002/ca.23006
Lokeshwar, S. D., Harper, B. T., Webb, E., et al. (2019). Epidemiology and treatment modalities for the management of benign prostatic hyperplasia. Translational Andrology and Urology, 8 (5), 529–539. doi:10.21037/tau.2019.10.01. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6842780/
Rawla, P. (2019). Epidemiology of prostate cancer. World Journal of Oncology, 10 (2), 63–89. doi:10.14740/wjon1191. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6497009/
Rider, J. R., Wilson, K. M., Sinnott, J. A., et al. (2016). Ejaculation frequency and risk of prostate cancer: updated results with an additional decade of follow-up. European Urology, 70 (6), 974–982. doi:10.1016/j.eururo.2016.03.027. Retrieved from https://pubmed.ncbi.nlm.nih.gov/27033442
Shoskes, D. A. & Zeitlin, S. I. (1999). Use of prostatic massage in combination with antibiotics in the treatment of chronic prostatitis. Prostate Cancer and Prostatic Diseases, 2 (3), 159–162. doi:10.1038/sj.pcan.4500308. Retrieved from https://pubmed.ncbi.nlm.nih.gov/12496826/










